Macular degeneration Tauhekenga uaua
Macular degeneration is the main cause of blindness and severe vision loss in Aotearoa New Zealand. It usually affects people aged over 50. It is often called age-related macular degeneration (AMD or ARMD). But there are also inherited forms that affect young people.
About macular degeneration
Macular degeneration is a disease that affects the cells that feed the back of your eye (retina). Because of the disease, waste products build up and form yellow deposits (drusen) in the central part of your retina (macula).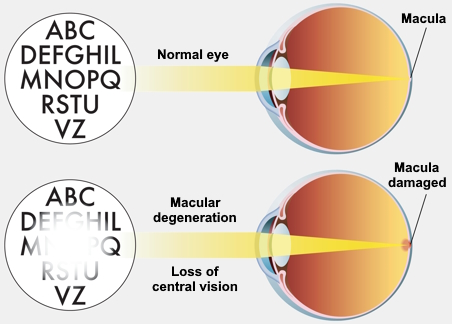
This causes a painless, progressive loss of central vision (what you see when you are looking straight ahead), but your peripheral or side vision (what you see around the edges) is not affected.
Types of macular degeneration
There are several types of macular degeneration.
Early and intermediate macular degeneration
This is where changes in your retina are milder, and you may get mild distortion or gaps in your vision. Distance vision and near vision are both affected. It progresses slowly and only affects your central vision. Your peripheral vision is normal.
Advanced macular degeneration – neovascular
This occurs when blood vessels grow under your retina. These blood vessels are fragile and leak blood, which causes scarring and loss of vision. The loss of vision can be sudden and needs immediate medical treatment.
Advanced macular degeneration – geographic atrophy
This causes a slow progressive loss of your central retinal cells causing a blind spot in your vision.
Causes of macular degeneration
We think it is caused by genetic and environmental factors working together.
People with a whānau history of macular degeneration are at increased risk, so it is important to get your eyes tested if your relatives have it.
Smokers have 3 times the risk of getting it and tend to get it 10 years earlier than non-smokers.
Less common types of inherited macular degeneration can affect tamariki (children) and young adults.
Symptoms of macular degeneration
If you have macular degeneration, you will have one or more of these symptoms:
- distortion, where straight lines appear wavy or bent or print appears blurred
- difficulty reading or doing anything that requires fine vision
- difficulty distinguishing faces
- dark patches or empty spaces in the centre of your vision.
You might also:
- need extra light to see
- be sensitive to glare
- notice you cannot see well at night
- be less able to distinguish between colours or contrasting objects.
If you have any of these symptoms, do not dismiss them as simply part of getting older.
Diagnosing macular degeneration
There is a test you can try yourself to see if you have macular degeneration. This is called the Amsler grid. The Macular Degeneration New Zealand website has this test, and instructions on how to complete it. The grid does not replace having your macula tested by an optometrist or ophthalmologist, particularly if you are aged over 50 or have any risk factors for macular degeneration.
Take the test — Macular Degeneration New Zealand
As well as the Amsler grid, there are other tests your eye specialist can do for macular degeneration.
Optical coherence tomography (OCT)
This is a scan of the back of your eye. It allows your optometrist or eye specialist to see what is happening in each layer of your retina.
Fluorescein angiogram
In this test, photos are taken of the back of your eye after a dye called fluorescein is injected into a vein in your arm. The dye travels to your eye where it highlights any abnormalities or damage to the blood vessels at the back of your eye. Your optometrist or eye specialist uses this test to investigate wet macular degeneration.
Treating macular degeneration
There are no medical treatments for early and intermediate macular degeneration, but our self care tips may help slow down macular degeneration and prevent vision loss in some people.
There are several medical treatments for advanced neovascular macular degeneration. They do not cure the disease but aim to stabilise your vision and maintain the best vision for as long as possible. In some people, the treatment can improve their vision.
- Medications called anti-VEGFs (for example, Avastin, Lucentis and Eylea) have been shown to control advanced neovascular macular degeneration.
- You are given these medications as an injection into your eye, and you may need them for the rest of your life. You and your eye specialist will determine the interval between injections.
There are currently no treatments for advanced macular degeneration with geographic atrophy.
Self care for macular degeneration
Although you cannot change your age or genetics, you can do things to decrease your risk of macular degeneration or slow it down if you already have it. Factors that may help slow the progression of macular degeneration include:
- not smoking
- eating fish 2 to 3 times a week, dark green leafy vegetables and fresh fruit daily, a handful of nuts a week, and limiting fats and oils
- maintaining a healthy lifestyle, controlling your weight and exercising regularly
- reducing your exposure to ultraviolet light by wearing sunglasses.
Some supplements containing lutein (a natural pigment found in lots of fruits and vegetables) help to slow the progress of macular degeneration in some people, although they do not improve it. These supplements may especially help people with moderate or severe dry macular degeneration.
Nutrition and supplements supporting eye health — Macular Degeneration New Zealand
These supplements are not publicly funded. You could ask your optometrist or eye specialist if they think you should try taking one of these.
Preventing macular degeneration
It is important to have your eyes checked regularly by an optometrist or ophthalmologist. This is especially important if you are over 50, as the risk of many eye disorders increases with age.
Everyone should have an eye health check at least every 2 years.
This content was written by HealthInfo clinical advisers. It has been adapted for Health Information and Services.